Background
Client: M. M.
- 27 year old male with C.V.A.
- Suffers from sensory deficits left side and apraxia
- Is undergoing acute rehab at Ghent University Hospital, Belgium
Posture assessment:
- Pelvic obliquity right
- Pelvic rotation left
- Posterior pelvic tilt
- Short hamstrings left
Mobility assessment:
- Uses foot propulsion right, combined with hand propulsion.
A clinical case by:
Lode Sabbe – Head of department Occupational Therapy at UZ Ghent – University Hospital Ghent
Bart Van der Heyden – Physical Therapist Private Practice ‘De Kine’ / SuperSeating
Carlos Kramer – International Educator Vicair
Ghent University Hospital – 2016
Problem
M. has to reposition himself constantly. Maximum sitting time without repositioning is approximately 5 minutes. M. also slides out of the chair due to foot propelling. After every movement, even if it’s short distance (5 meters), he has to reposition himself.
To help M. with these problems, it was tried to train him to contain a better sitting posture in the wheelchair. M. is still hopeful that he will walk again after his rehabilitation process. Because of M.’s idea of walking again in the future, his wheelchair use is not optimal, but he does not care. The chances of M. walking again in the future are very small, but he does not want to believe this. Therefore the problem of sliding and repositioning continue to stay the same.
Solving the problem
With iShear we now have a tool that can show what is happening with the Total Shear Force in the seating system (TSF) during the day. The TSF can be a factor that causes M. to slide out of the chair.
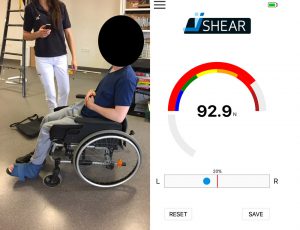
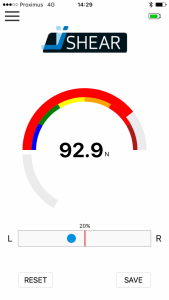
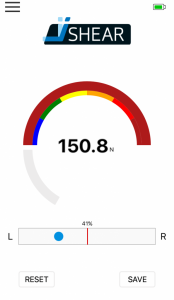
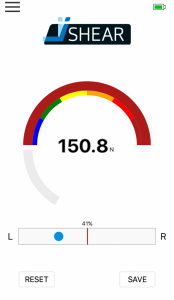
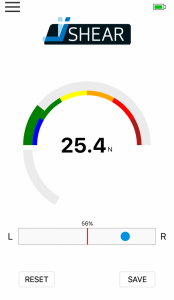
We did a baseline measurement, to see what the TSF is in his normal resting position:
Then we changed his wheelchair set-up and we measured the TSF again.
We did two interventions:
- Add a better lumbar support
- Add a better thoracic support
With the extra support we see a decrease of TSF. Less TSF can result in less sliding.
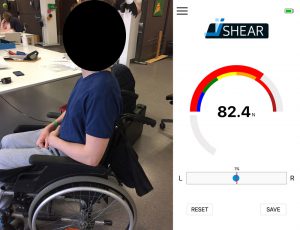
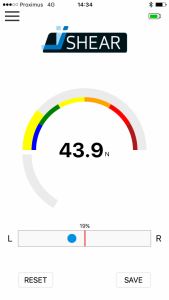
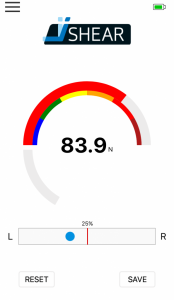
We also looked at his way of propelling and measured the TSF during movement.
After measuring his baseline, we taught him a new way of propelling and showed the differences in TSF with the iShear app.
We see an increase of 15 Newton in TSF due to movement. More TSF makes it more likely that M. will slide.
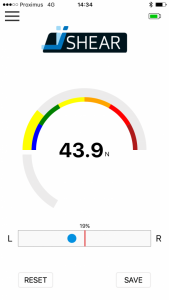
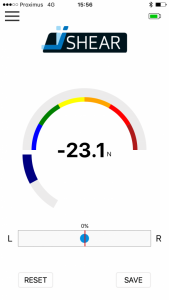
We taught M. a new way of moving, now in a more upright position with less or no resting against the back support during propelling. Due to his apraxia it took him a while to familiarise himself his new way of moving. After some practice we measured his TSF.
Results
If we look at wheelchair set-up interventions, we decreased the TSF with 40 Newton (92,9-51,9).
The extra support we added was temporary. M. needed a new wheelchair to make this a permanent set-up. During the day M. stayed in his current wheelchair with the extra support and he had the feeling he needed less repositioning. Observation of M. showed less need for repositioning.
M.’s found this new propulsion technique hard to maintain. We asked the therapist to monitor M. and train him in this new technique.
Conclusion
M.’s new wheelchair set-up is better for his posture and better if we look at the TSF. M. is now waiting for a new chair with the adaptability that he needs. The iShear was a helpful device in showing the TSF in different wheelchair set-ups. With the iShear we had a tool to show us the decrease of TSF in new wheelchair set-ups; the less TSF, the more likely it is that we will increase seating tolerance (time sitting in chair without repositioning). With the iShear app we could also show M. what the different results were with different wheelchair set-ups.
Outcome over time
M.’s found the new propulsion technique too tiring. Although he had had an insight into the effect of his old technique M. didn’t continue to use the new technique. We think this is the result of his apraxia in combination with his hope of being able to walk after his rehabilitation.